
Following several abstract presentations at ATS Conference 2023, we have asked Julien Guiot - Head of Clinics at CHU Liège, Belgium and Associate Professor at ULiège - to comment on their recent studies in the field of imaging-based biomarkers in vascular lung diseases.
Prof. Guiot is managing the team of interstitial and vascular lung disease in CHU Liege. He leads the research team and collaborates with expert partners in the field to identify new ways to phenotype patients with respiratory diseases with the help of CT scan imaging and quantification.
Having initially studied biological and translational evaluation of patients, the team moved on to new imaging-based markers, since the COVID-19 pandemic. At this point, they have started to work with AI-based models in collaboration with clinicians and clinical decision support systems. While working on interstitial lung diseases (ILDs), the team focuses mainly on idiopathic pulmonary fibrosis (IPF) and systemic sclerosis (SSc) patients, trying to merge these two conditions with progressive pulmonary fibrosis.
For the past two years, they have been working with Thirona’s AI-based lung quantification platform LungQ, applying its artery-vein phenotyping algorithm (LungQ AVX) in their studies. The first results are very promising, showing that the AI-enabled analysis could potentially allow for early detection of pulmonary vascular abnormalities and can contribute to a variety of associated diseases, by timely initiation of the treatment planning.
Addressing the challenges of pulmonary hypertension treatments
Pulmonary hypertension (PH) is a general term used to describe high blood pressure in the lungs from any cause. According to the WHO classification, there are 5 groups of PH based on different causes (Figure 1). It is a condition associated with high comorbidity, especially when accompanied by other lung diseases, and the diagnosis of the potential cause is often difficult to conclude. PH (group 3) appears quite frequently in combination with ILDs or severe chronic obstructive pulmonary disease (COPD).
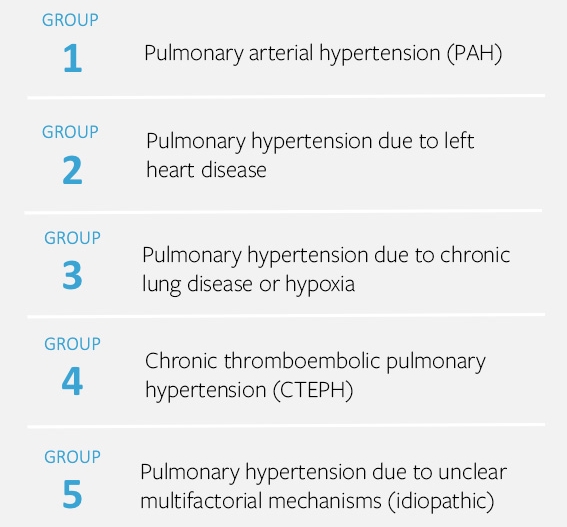
Figure 1: PH classification according to the World Health Organization
According to Prof. Guiot, one of the major challenges that clinicians face is to identify and phenotype PH patients early on. “Until now, we haven’t been able to treat PH associated with lung disease due to lack of a proven and efficient therapy. However, very promising specific therapies have emerged recently, that can specifically target this group”, says Prof. Guiot.
When it comes to pulmonary arterial hypertension (PAH, group 1), for example – it can also be found in patients with SSc or other connective tissue disease. In addition, it can come with other conditions like congenital heart diseases, HIV or cirrhosis, it can be drug induced or inherited, as well as be present in patients with no specific pathobiological process identified (idiopathic, group 5 ). Prof. Guiot elaborates: “The bottleneck here is firstly to identify the patients at the earliest possible stage and secondly to determine whether it is the pulmonary arterial hypertension (group 1), as only these patients can benefit from specific vasodilator therapies (except for group 4). However, the distinction between PH group 1, 2 and 3 can also be a challenging matter.”
Anno 2023, it is still quite difficult to make an accurate and timely diagnosis, due to comorbidities associated with PH. The diagnosis is based on an invasive hemodynamic evaluation, taking place when the symptoms are already severe. Artificial intelligence (AI) demonstrated the potential to offer a way to identify PH patients with the use of lung CT imaging, which was the starting point for the collaboration of CHU Liege with Thirona.
Treatment paths and the potential of CT imaging for pulmonary vascular diseases
Based on the medical symptoms, and the presence of other conditions forming potential risk factors, patients with suspicion of PH may be initially referred to either a lung or a heart specialist. Generally, it would initially be a GP to refer such patients to a CT scan. However, since they cannot perform echocardiography, the patients are referred to a specialist for a further evaluation.
Today CT is used as a baseline assessment of PH. When assessing the possibility of PAH (group 1) CT is used to confirm that the patient is not suffering from extended lung disease. For SSc patients, CT is a frequent procedure to exclude ILD which forms a higher risk for these patients. In very severe forms, they can also suffer from PH due to chronic lung disease or even develop PAH due to specific vascular involvement linked to this pathological condition. According to Prof. Guiot: “It’s clear that having a tool that could be used to evaluate CT scans of patients with risk of developing any type of PH could be of high interest for clinicians.”
”Considering the promising results of trials like the INCREASE trial, it can be expected that in the course of upcoming years, we should be able to treat patients with group 3 PH.”, prof. Guiot continues. “It will be very important to have the ability to identify those patients at the earlier stage of the disease, in order to apply the most appropriate treatment and to maximize the therapy effectiveness. Especially if we could enable analysis merging the lung fibrosis and PH conditions, like it is being done with systemic sclerosis patients for evaluation of PH and ILD. ”
Looking forward, having clinicians perform CT at the baseline evaluation in case of an unexplained dyspnea, we already have a great starting point for image analysis with use of AI. “If we had an AI model that would automatically analyze and assess the scans, it would be a major step forward for the early identification of PH”, says prof. Guiot. CT could be possibly included in specific evaluations next to hemodynamic assessment in clinical trials. In fact, there are already many trials conducted on group 3 PH. As those patients with COPD or ILD already have CT follow-up evaluations, this could be a way to have data over time coming from clinical trials. This kind of information could help convince clinicians that disease is somehow associated with the prediction of the patient's outcome or with the treatment response.
Research with LungQ AVX (Thirona). Main takeaways.
With his experience in the field and his work with Thirona for 2 years now, we have asked Prof. Guiot’s conclusion on the current state of AI and Thirona’s software specifically. “ I believe that AI has an incredible potential to enable major improvements in treatment of PH, specifically when it comes to identification of patients with P(A)H. Having an invasive hemodynamic catheterization as the gold standard, we are also evaluating the correlation between vascular biomarkers and hemodynamics. If we can confirm that the combination of symptoms, echocardiography (ECG) and CT could aid us in a more accurate diagnosis of patients at risk of P(A)H, we could transform the way it is diagnosed today and show that it could be less invasive and could help as a clinical decision support tool.
If we can show the correlation between hemodynamics and vascular biomarkers, AI-based imaging markers could become a companion tool for clinicians, acting as a closer non-invasive follow-up in parallel to hemodynamics. Moreover, it would enable non-expert clinical centers to triage and identify PH patients early on, directing them to the appropriate specialist for further evaluation.”
As rigorous studies with multiple research partners continue, we are excited to see novel findings being discovered with the use of Thirona’s AI technology, potentially enabling groundbreaking innovations in the treatment of complex diseases like PH. We would like to thank Prof. Guiot for sharing his work and experience with exploring the potential of AI and Thirona’s LungQ AVX analysis in identifying new ways to phenotype patients with pulmonary vascular diseases.